Transitioning from the fee-for-service reimbursement system to a value-based care structure creates huge financial challenges for health systems. Providers must deliver better outcomes for less money to thrive and figure out a way to improve revenue streams. Lower hospital readmits and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores drive Medicare reimbursements, fueling the need for hospitals and physicians alike to improve outcomes and revenues.
Focus on the Patient
In an article published in The Harvard Business Review in 2013, “The Strategy That Will Fix Health Care,” Michael E. Porter and Thomas H. Lee, M.D. make the case that patient concerns and value-based care should drive quality measures: “It is not surprising that the public remains indifferent to quality measures that may gauge a provider’s reliability and reputation but say little about how its patients actually do. The only true measures of quality are the outcomes that matter to patients. And when those outcomes are collected and reported publicly, providers face tremendous pressure—and strong incentives—to improve and to adopt best practices, with resulting improvements in outcomes.”[1]
Keeping a patient out of the hospital within the 7- or 30-day readmission window is a huge consideration. It requires a focus on preventative healthcare versus reactive. Getting patients to actively engage in their own care and rehabilitation plays a big role in achieving lower readmits. Patients who have an easy-to-use tool that gives them clinical-grade feedback about their condition, and instructions on what to do next are more likely to be engaged in their care. This, in turn, improves outcomes and patient satisfaction. Happier patients are more likely to give higher marks to a hospital on the HCAHPS survey, which in turn, positively affects reimbursements. And so it goes.
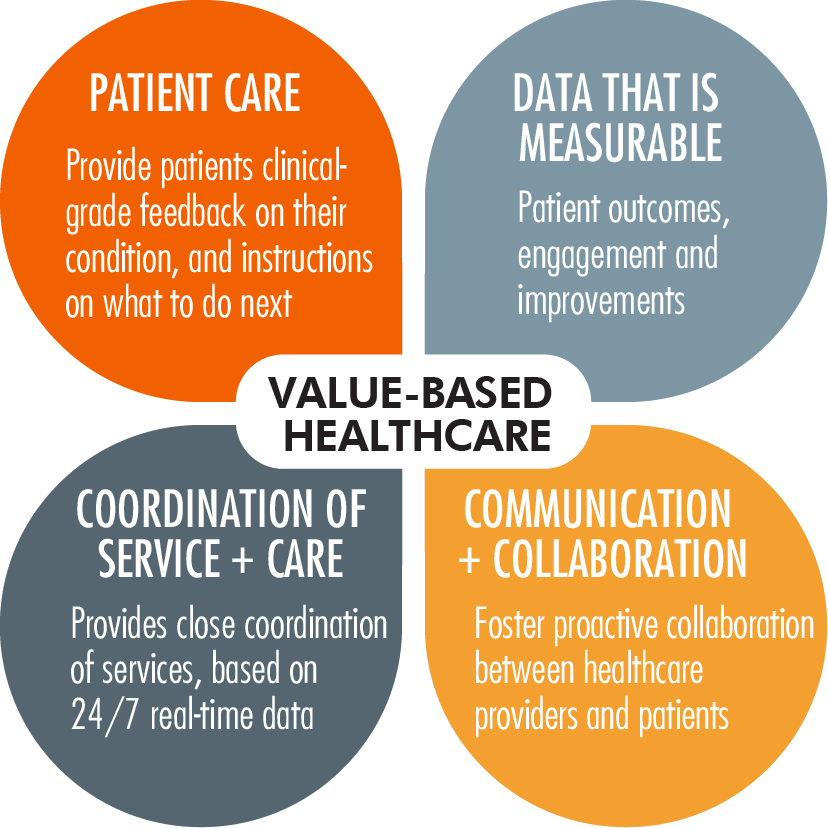
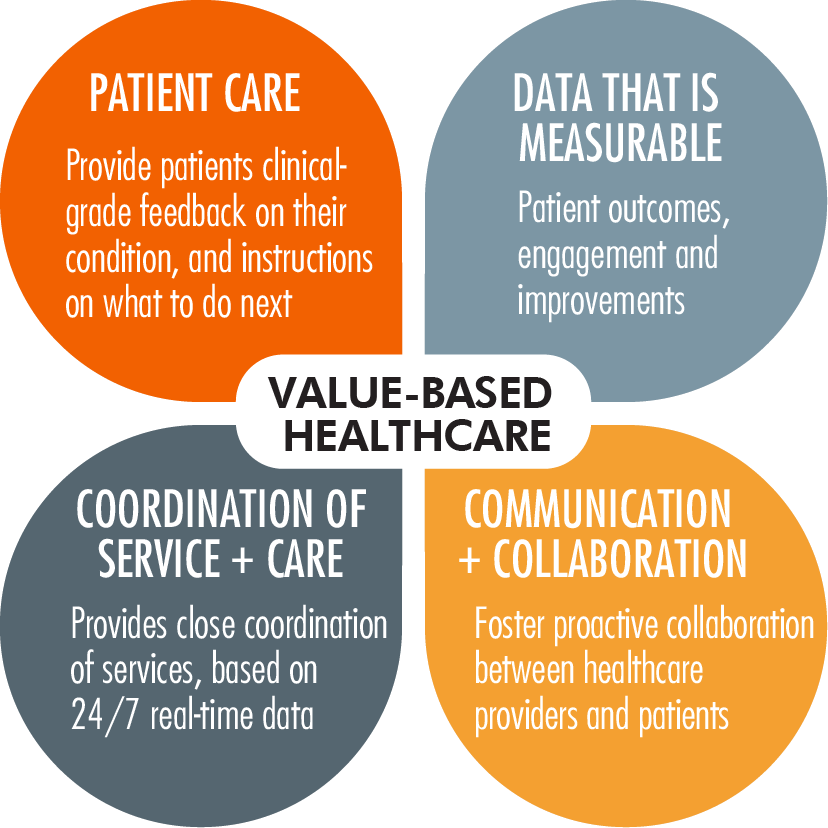
Value-based healthcare infographic
Tech Innovations Can Help
In order to integrate a value-based care system doctors and hospitals need access to easy-to-use tools for patients and they need a way to bill for those services. Finding the right, medically relevant products that can measure results and fit in with current billing practices is key. One example is cardiac remote patient monitoring solutions.
Cardiac remote patient monitoring is currently monopolized by a handful of companies who aren’t progressing. Unfortunately for patients, outdated Holter and Event Loop monitoring systems are still being used, with bulky devices that don’t provide real-time updates to physicians. Innovations within remote cardiac monitoring are providing a way to engage patients in their own care via real-time access to their conditions. Biotricity has developed a remote cardiac monitoring device that detects arrhythmias and sends an immediate alert to a 24-hour monitoring center, which in turn contacts the patient to offer assistance. Access by physicians and patients to real-time data increases the quality of care, engages patients and potentially lowers their risk, lowers hospital readmits and hits to reimbursement rates.
Gain control and improve revenue streams
Improved outcomes allow you to comply. Making a profit allows you to compete. Biotricity uses an in-source business model that allows you to prescribe our monitoring device and provide it to your patients while they’re in your office. This model allows you to reap the revenue benefits. Our solution is insurance reimbursable because we purposely built our solution around existing billing codes.
This makes it easy for your practice to bill for the device.
Innovations that deliver better outcomes and improved revenues will play a factor in thriving in the value-based healthcare world. Make sure your practice isn’t left out.
_________________________________________________
[1] https://hbr.org/2013/10/the-strategy-that-will-fix-health-care